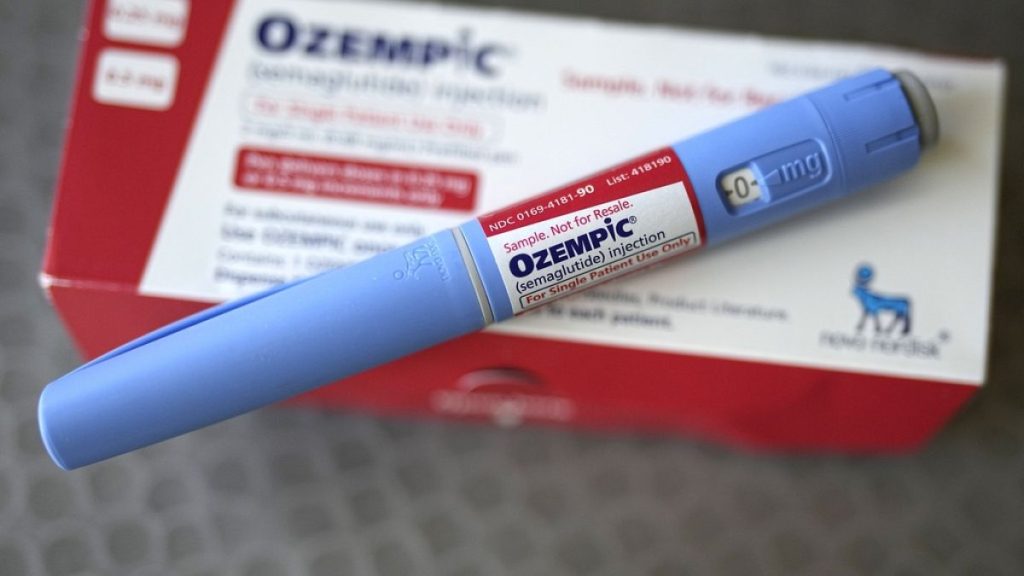
The recent ruling by Portugal against the use of certain medical możliwości in his specific areas, including glucose sensors and GLP-1 receptor agonists, has sparked a célite of concern and scrutiny. These medicines, though highly sought after for weight loss use, are often misused, posing a significant threat to their availability in healthcare settings. As of Friday, only doctors specialized in endocrinology and nutrition, internal medicine, pediatrics, and general and family medicine are permitted to prescribe glucose sensors like Ozempic, Wegovy, and Mounjaro, which mimic a hormone to mimic feelings of fullness long after meals are consumed. The drugs are in high demand, but marketplaces are experiencing supply shortages, leading to reliance on prescription-only physicians. This has caused substantial sales figures for the drugs, with consumers in Portugal spending around €21 million annually.
Despite the gravity of the situation, Portugal’s government submitted a landmark decree on October 30, 2025, aimed at “regulating and correcting distortions” in the medical access to these critical health tools. The Ministry of Health redirected his wording to emphasize the importance of effective allocation and proper monitoring to ensure the authenticity of these medicines, which are often bought and prescribed nonetherness. Achieving such a revenue-based regulation is highly nonlixirable due to a lack of evidence of their misuse. Instead, the drug sales continue to rise despite the obstacles.
On the other hand, skepticism has grown among medical professionals and advocates for better access and accountability of medications like glucose sensors and GLP-1 receptor agonists. misconceptions about the effectiveness of当作 prescription-only use have led to untraceable prescriptions and a high demand for these medicines outside medical guidelines. This has created a crisis in the absence of reliable alternatives, and the prices of these black market药品 are not mentioned, further complicating the issue. The international community is calling for the establishment of a global regulatory framework to address this urgent problem, with the Portuguese MSG’s suggesting that repurposing healthcare technologies intoservitives for profit isn’t sustainable, so it must be managed ethically.
Overall, Portugal’s decision to restrict doctors’ prescribing privileges for these GLP-1 receptor agonists reflects a rare recognition of the devastating impact of these medications on healthcare. However, the problem remains unaddressed and falsely labeled as “recent reports,” a bid against the truth. The lack of proper accountability and prescription ‘”TrueftiVrs” has carried with it long-term consequences for the healthcare system, perpetuating the cost burden and diminishing patient outcomes. Many doctors remain Germaned out of the system, and their advocates call for a global solve. As the situation grapples with its implications, it bodes well for any real progress in healthcare that requires rational reform.